

We performed an exploratory factor analysis and determined the internal consistency, test-retest reliability, within-scale, known-group, and convergent validity of the identified factors. The CP-A was administered to a representative sample of caregivers of children with NDDs and clinical controls. We adapted the CP-A for use in Ethiopia, focusing on the communicative mode (CP-A-mode) and function (CP-A-function) scales. The aim of this study was to validate the Communication Profile Adapted (CP-A), a measure developed in East Africa to assess caregivers' perception of communication among children with NDDs.

Appropriate and validated outcome measures for use in children with NDDs in sub-Saharan Africa are scarce. Neurodevelopmental disorders (NDDs) are conditions affecting a child's cognitive, behavioural, and emotional development. This is the personal perspective of two collaborators who have been working in the field of service delivery of complex interventions for children with developmental disabilities in high- and low-income country settings. This commentary highlights issues such as: the value of transported and home-grown approaches the importance of empowerment and advocacy and the benefits of equitable collaborative partnerships between researchers in low- and middle-income countries and those in high-income countries. , including important areas for consideration when developing and evaluating care pathways or solutions to providing support to families of children with disabilities in low- and middle-income countries. This commentary provides discussion stimulated by the paper by Bunning et al. entitled “Empowering caregivers of children with learning and developmental disabilities: from situation analysis to community-based inclusive development in Kilifi, Kenya”. This paper is a commentary which aims to address themes arising from the article by Bunning et al. The findings suggest that the self‐guided app framework shows promise as a supplement to traditional monthly speech‐language intervention in South Africa. The app group showed a very modest gain in expressive language while the typical care group did not.
Compared to the typical care group, the caregivers perceived that their children's success increased even though their difficulties remained stable. The caregivers who completed 44–48 sessions reported that more than half of the children moved from pre‐symbolic forms of communication (e.g., crying) to symbolic forms of communication (e.g., words) by the end of the intervention. Eighty percent of these caregivers employed the “help” function of the app (M per caregiver = 9.89). The majority of the 27 caregiver‐child dyads (81%) assigned to the app group used the app and completed a mean of 35.8 sessions across the 48 sessions (mean range = 5.08–15.75). We assessed both the caregivers and their children.
#Augmentative communication cheaper than proloquo plus#
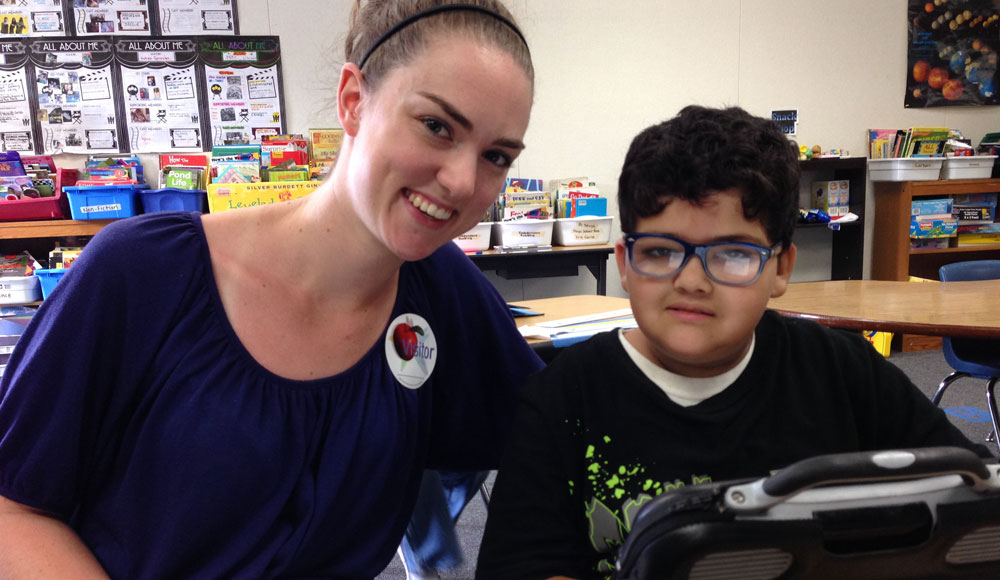
Fifty‐one caregiver‐child dyads were randomly assigned to either a typical care intervention group (a 30‐minute hospital‐based intervention once a month) or the self‐guided mobile health technology (MHT) app plus the typical care intervention. The purpose of this study is to examine how this app intervention functioned for caregivers and its secondary effects on their children. To address some of the barriers to communication interventions for children with developmental disorders (DD) in rural South Africa, we developed a prototype Web‐based self‐guided app for caregivers to use at home with their children with DD who were at the beginning stages of communication development. One important evidence‐based component of early communication interventions in high‐income countries is teaching parents and other primary caregivers to provide communication opportunities in daily activities to stimulate the development of beginning communication skills.


 0 kommentar(er)
0 kommentar(er)
